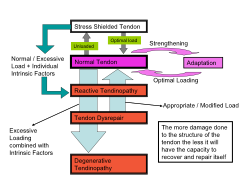
There is now an increasing recognition that tendons react to a variety of factors, some mechanical (external) and some personal (internal) factors. The following is a non-exhaustive list of some of these factors
There are different types of pressures / loading that affect tendons – and that affect may be either Positive or Negative.
1. Tensile – good to maintain fibrous tissue in tendon
2. Compression – good to maintain junction with bone
3. Friction – gliding adjacent tissues / paratendon
4. Combined types – forms and maintains bone spurs
A normal healthy tendon is able to cope 1- 3 of these but is less well able to cope with the last type of stress
Adjusting the loading on the tendon depends on :
- Load type - as above
- Position,
- Muscle length,
- Contraction type - load increases through static, concentric, eccentric
- Eccentric load can help to strengthen dysrepaired or degenerative tendons but is not suitable for reactive tendons.
The Highest Tension Loading occurs on a tendon during:
- Eccentric (muscle getting longer as working ) contraction of muscle
- Rapid contraction of muscle
- High resistance / weights being moved by muscle
- Repeated (pre) Stretch – Shorten Cycle in muscle activity
- Application of high loads should be done slowly at first, more quickly later.
- Reduce loading at increased length
- Minimise compression of the injured tendon
High tension loading is more damaging when combined with compression.
Compression alone is the least damaging type of loading on tendons.
Long Tendons are prone to overloading in the middle.
Force on the tendon is greater when the muscle is holding a load while stretched.
Short tendons are more prone to overloading at either end at their attachments (insertions) to bones.
Tendon pathology is most likely to develops when tendons are exposed to repeated stretch shorten cycles when the muscle tendon complex is already pre-stretched. Back to Top
Extrinsic Factors
- Training errors
- Time (duration)
- Distance
- Repetitions (intervals)
- Intensity
- Hills
- Surfaces
- Hard Vs soft
- Canted road
- Shoes and equipment
Intrinsic Factors
Age
Female – post menopause
Diabetes
Obesity e
Alignment abnormalities
Foot over Pronation / Supination
Muscle weakness / imbalance
Flexibility
Previous injury (strain, sprain
Tendonopathy is a term used to describe a range of injuries that affect tendons. It can apply to acutely injured tendons (inflammation = tendonitis) or to those tendons that are dysrepaired + degenerated (tendonosis) but not inflamed.
Injured tendons are ‘staged’ on a continuum of progressive deterioration from acutely injured to the worse case scenario where the tendon snaps, or ruptures.
The most common sites where it occurs are the Achilles tendon (AT) at the ankle, the patellar tendon (PT) at the knee, the supraspinatus tendon and other rotator cuff tendons at the shoulder and the common tendon of the wrist extensors + flexors at the elbow - tennis and golfers elbow respectively.
Acute tendon injury has simple mechanical tearing of some tendon fibres, leading to an inflammatory response, proliferation of tendon cells and ground substance leading to either full repair + healing, or to poor repair / failed repair which is called dysrepair. Where full repair does not occur the risk of re-injury was greatly increased.
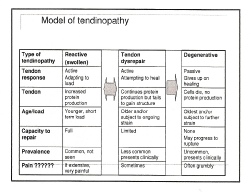
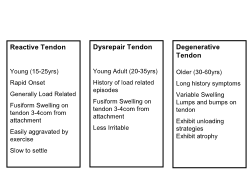
This model of tendonopathy proposes a progressive deterioration from reactive tendon on initial injury through to tendon dysrepair to degenerative tendon.
Tendons tissues adapt / respond slowly to rehabilitation.
The tendon needs up to 4 days to respond to training, especially to high loading . Therefore high load training cannot be done daily during early rehab but must be spread over a prolonged period of time (> 4 weeks).
Rehabilitation will depends on:
- The amount of pain arising from the tendon
- The stage of Tendonopathy.
Reactive tendons need to be calmed down
- Avoid eccentric work / loading
- Decrease / alter loading – heel raise, elbow strap
- Manage inflammation symptoms
Dysrepaired Tendons need to be stimulated to restore good structural tissues / normal tendon structure
- Possible concentric and eccentric loading
- Avoiding aggravating factors
Degenerative Tendons need to be stimulated to make the healthy parts of the tendon as strong as possible
- Strengthen the whole muscle tendon complex
- Manage biomechanical loading and internal factors as much as possible.
Rest - means where the tendon is relatively unloaded. It is
- Not good for tendons
- Provides no stimulus for protein or structural fibre production
- Provides no maintenance for muscle tendon unit capacity
- Provides no maintenance of musculoskeletal capacity
Adjusting the loading on the tendon is achieved by altering
- Load type – position,
- Muscle length,
- Contraction type
Eccentric load can be used to strengthen a damaged tendon but is not suitable for use with reactive tendons. During eccentric activity ensure
- Slow / gentle application of load.
- Reduced energy storage and release within sessions
- 2 days between high loads sessions
- Reduced loading at increased length
- Minimise compression at the attachment to bone
- Plan high (strength), Medium (energy storage), Low(power) loading days
- To avoid excessive unloading / avoiding load not good either
Tendons that were previously injured should not be allowed too much ‘time off ‘ training – i.e. during the off season, rest for other injury etc. These tendons are less well able to cope on resuming normal training and will break down again if they are not protected by on going training to maintain its load tolerance capacity.
High Load Rehabilitation should begin with training on every third day.
To increase the tendons strength apply slightly higher loads than those normally experienced during daily activities on the training days. Increase to alternate day training. Aim to move through from static loading, to concentric loading (muscle shortening) and finally to eccentric loading (muscle lengthening) of the tendon.
Aims
- Unload the Tendon initially, later manage the loading
- Get Strong – address muscle weakness
- Static / slow tendon loading during early rehab
- Progress speed of activity
- Progress volume of functional activity
- Apply elastic loads in final rehabilitation
1st Stage – Strengthening
0-3 months, Exercises 1 – 2 x daily
Using
- Isometrics / very slow concentric / eccentric contraction
- Sustained loads in inner ROM (30-60 secs x 4-6 reps)
- Avoiding tendon compression
Progress as tolerated
2nd Stage – Functional Strengthening
2 – 4 months, Exercise on alternate days
Using
- Slow concentric / eccentric contraction
- Moving loads into middle + outer functional ROM
- Increase resistance / load in weightbearing – use speed
- Increased emphasis on eccentric later
- Mostly low and medium loading used
- Build muscle endurance
- Progress as tolerated
3rd Stage – Speed
- Increase speed on every second or third day.
- Speed significantly increases load
- Continue with similar exercise faster
- Control ROM
4th Stage – Athletic Function
2-3 months, Schedule high and medium load days
- Increase the speed of loading
- Sport specific activities
- Capacity to absorb repeated elastic loading
- Propulsion activities
- Repeated concentric-eccentric activities (hopping, skipping)
- Acceleration – deceleration, change of direction
The PDF file below is a scholarly paper assessing the the relative benefits of differing loading programmes for Rehab of Achilles and Patellar Tendonopathy in the lower limbs. Back to Top
Seek coaching advice on sport technique
- Racquet Sports
- Throwing Sports
- Gripping / paddling
- Running gait
Walking gait - podiatrist
Footwear
Coaching - Biomechanics Correction

‘Tennis elbow’ is a generic term used to describe a tendonopathy which is an overuse injury of the tendons at the outside of the elbow. It may also be called lateral epicondylitis or as a tendonitis if the injury is acute / recent
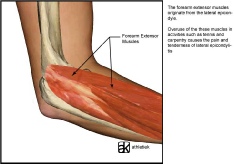
‘Golfers elbow’ is a similar condition affecting the tendons on the inside of the elbow and is also called medial epicondylitis.
Neither is necessarily associated with playing tennis or golf but more with the excessive use of the muscles attached to the bone at the elbow - the wrist extensors affecting the outside and the flexors affecting the inside of the elbow..
It occurs where there is excessive repetitive activity, excessive gripping with the hand or working with the hand in an awkward / poor ergonomic position.
Epicondylitis  or tendonitis around the elbow responds well to treatment by physiotherapists.
or tendonitis around the elbow responds well to treatment by physiotherapists.
Assessment will determine what the key causative factors are and how they have led to the development of the condition.
Treatment may include:
- Avoiding the provoking activity for a short period
- Soft tissue massage
- Exercises for stretching and strengthening of the affected muscles and other tissues
- Adjusting work and playing postures, adjusting sports equipment Electrotherapy Modalities
- Medications - prescribed by a GP
- A support brace can be worn over the upper part of the affected tendon. This relieves some of the strain + allows ‘rest’.
For a detailed assessment and advice or treatment contact us at Ennis Physiotherapy Clinic.
Tennis / Golfers Elbow
 The shoulder joint has a large range of multi directional movement in many planes. Joints that are highly mobile tend to be more unstable. To achieve a high mobility the shoulder depends more on dynamic stability from the rotator cuff muscles around the joint than on the static stability from ligaments.
The shoulder joint has a large range of multi directional movement in many planes. Joints that are highly mobile tend to be more unstable. To achieve a high mobility the shoulder depends more on dynamic stability from the rotator cuff muscles around the joint than on the static stability from ligaments.
Another factor affecting normal shoulder function are position + movement of the shoulder blade, swelling of the AC joint and the shape / orientation of the acromion (bony point of the shoulder).
These affect the risk of developing tendonitis or impingement at the shoulder. Tendons around the shoulder form the ‘rotator cuff’
Tendonitis of the rotator cuff tendons of the shoulder is a common cause of shoulder pain. It is frequently due to overuse (repetitive) or over exertion. It can occur as a secondary issue to poor posture in older people with slouched postures. Repeated use of the arm, at or above shoulder level, can provoke inflammation. A fall onto the hand or elbow or a sudden drag on the shoulder / arm can also provoke acute symptoms.
 Impingement of the tendon can occur at the shoulder between the head of the humerus and the acromion during vigorous, repetitive activity at or above shoulder level.
Impingement of the tendon can occur at the shoulder between the head of the humerus and the acromion during vigorous, repetitive activity at or above shoulder level.
The usual movements that cause impingement are a combination of forward flexion to 900 and inward rotation of the arm. Swimmers, throwers, racquet players etc are all at risk.
In older people there are changes within the acromion, the ligaments around the shoulder and the position of the scapula which increase the risk of impingement. The tendons can become inflamed, swell and sore. If this becomes chronic it can cause scarring, weakness and then tearing.
This condition, if chronic, may lead to significantly reduced movement and pain, ultimately possibly ‘frozen shoulder’. It responds slowly but well to conservative treatment including exercise and joint mobilisation. Increased strength, good flexibility of the muscles around the shoulder and postural retraining all help to improve things in the longer term.
For further information and an assessment please contact us at the clinic.
The following video gives an indication of some of the possible exercises that may be suitable for someone with shoulder + rotator cuff problems. An alternative video which has some more basic exercises and an explanation is at this link. These links are for information only and specific advice should be sought from your chartered physiotherapist. Back to Top
Shoulder Tendonitis / Impingement
Treatment can be provided at Ennis Physio Clinic
Treatment is primarily aimed at restoring the tensile strength of the tendon to that of pre injury levels.
Where inflammation is present it must be controlled and reduced.
In the acute phase use the RICE regime.
Gradually increase the loading on the tendon during activity once pain is controlled.
Simple heel raises both concentrically and eccentrically - slowly - are begun as soon as possible and integrated into normal functional activities.
Slow heel raises are progressed to rapid heel raises, rapid alternate heel raising, hopping, skipping and then jumping.
Gait re-education practice without a limp is to be achieved prior to progressing to walking fast, striding, jogging, running and jumping.
Acceleration is practiced in a controlled manner - changing walking and / or running speeds.
A variety of walking and running drills are available if needed.
Treatment duration will vary depending on severity of injury and the demands you intend to place on your healed tendon.
The following video gives an indication of some but not all of the treatment possibilities. Please note reference to Physical Therapy I/ therapists n the USA is the equivalent to a Chartered Physiotherapist in Ireland.
.
I recommend, when doing the exercise shown on the step in the video below, that you start by not dropping below the level of the step (or indeed begin by doing this exercise standing on the floor before progressing to doing it on a step).
Treatment of AT Injury
Achilles tendon injury is frequent + occurs in all populations. An acute tendon injury is inflamed and is called a tendonitis. A more chronic injury, where no inflammation is present, is referred to as a tendonosis.
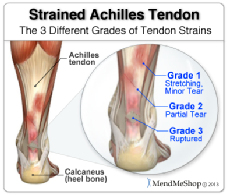
Overuse tendonopathy is associated with gradual onset of pain and morning stiffness after an increase in activity. Symptoms diminish with activity but return after rest. Heat is reported to alleviate symptoms.
Acute symptoms is associated with partial tears or rupture of the tendon. In the latter people often report being kicked on the heel / tendon and of hearing a loud ‘shot’ like noise. There is often thickening of the tendon and sensation of a ‘creaking’ during movement.
O ther things to consider are foot mechanics, tight calf muscles, weak calf muscles, poor balance, stiffness at the joints of the ankle + foot and an ability to single leg heel raise / hop.
ther things to consider are foot mechanics, tight calf muscles, weak calf muscles, poor balance, stiffness at the joints of the ankle + foot and an ability to single leg heel raise / hop.
Injury in sports people is often associated with changes in intensity of training or sudden increases in training loads.
In the general population it may be associated with sudden changes in general activities or in footwear - a change to little or no heel or support / walking barefoot (as in when on holidays).
Achilles Tendonopathy/ Tendonosis




Mon - Fri 9.30am - 8.30pm


3A Barrack Close, Barrack St., Ennis, Co. Clare V95 X437

065 6840757
| Health+Safety Services |
| Sports Clubs+Teams Services |
| Standing Posture |
| Sitting Posture |
| Childhood Posture |
| Using Portable Devices |
| Normal Walking |
| Running |
| Running Drills Videos |
| Muscle Energetics |
| General Fitness |
| Losing Body Weight |
| Gaining Body Weight |
| Weight Loss Programmes |
| Start to Run |
| Start to Swim |
| Start Cycling |
| Start Nordic Waliking |
| Rehab of Tensdons |
| Loading of Tendons |
| Non Specific LBP |
| Posture |
| Intervertebral Disc |
| LBP Treatment |
| Non Specific Neck Pain |
| Neck Care Advice |
| Hamstring Strain |
| Ankle Sprain |
| ACL Injury |
| Joint Replacement |
| Shoulder Dislocation |
| Tennis Elbow |
| Wrist fracture |
| Fractured Knuckle |
| Selecting a Racquet |
| Racquet Grip Size |
| Racuet Sport Injuries |
| Training for Racquet Sports |
| Ski + Board Injuries |
| Injury Videos |
| Injury Prevention |
| Preventing Injury in Musicians |
| Irish Dancing |
| Preventing Dance Injury |