The hamstring muscles are frequently injured in sporting activities.
Usually it is injured at the end of the leg swing, during kicking actions, or during accelerating at the start of sprinting.
Hamstring muscles have a number of functions including pelvic positioning / posture and preparing the limb for loading during walking and running. It extends over two joints - the hip and knee. It is largely a postural muscle and so not best suited to very high intensity activity.

Risk factors for injury include:
- Previous injury
- Increased tightness in muscle
- Age
- Reduced flexibility
- Reduced Strength
- Low Back Pain
Muscle Injury Severity
All muscle injuries are graded to give an indication for severity and to help direct treatment / prognosis / gauge return to sport
- Grade I - small number of fibres affected, causes localised pain but no loss of strength
- Grade II - affects significant numbers of fibres, causes pain, swelling and pain on use of muscle with associated loss of strength and flexibility
- Grade III - Complete tear of the muscle, usually at the junction between muscle and tendon

Treatment
- RICE regime
- Activity:
Without pain in shortened position, including static work, gradually increasing in ROM + intensity
‘Activation’ of the core
Separate + combined lumber movement and leg movements
Dynamic jogging / running without pain or limp
- Technical drills: sidestepping, hurdle walk over, sumo walk, lunge, high knee walk, heel flicks.
- Gentle Stretching of hamstrings starts after 5 days
- Strengthening programme – general and sport specific
A sprained ankle ligament occurs when the foot is twisted
severely, usually turning inwards under the leg, either when
turning suddenly or landing on uneven ground.

There is often severe pain, immediate swelling and variable amounts of bruising.
If pain on walking or putting weight on the foot persists an X-Ray may be needed to exclude a fracture.
Repeated sprains of the ankles may lead to joint instability and poor balance and co-ordination. Exercises to prevent this should be included in the rehab programme.
Treatment can be provided by contacting us and includes
- RICE Regime
- Proprioceptive support taping / strapping
- Relative rest / reduced activity
- Functional Rehab: jumping, turning, ball drills
- Balance Board exercises
- Calf strengthening
- Progressive jogging / running / jumping / kicking

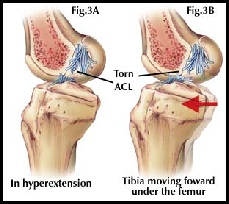
The Anterior Cruciate Ligament is a key stabiliser of the knee joint.
It prevents the knee from bending backwards (hyper-extension) and from bending sideways to the inside too far.
Injury to this ligament is very common in sports that require a lot of pivoting on one leg while changing direction, or where direct contact forces the knee backwards or inwards.
Female athletes are much more at risk of injury when playing or competing at the same level / intensity as their male peers. This is due to the differences in anatomy - the increased inward slope of the thigh bones making females more ‘knock kneed’.
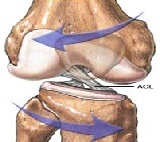
If the ACL is ruptured it leaves the knee unstable and exposes other tissues to increased risk of injury too. It is common to surgically reconstruct the ACL
A long period of Rehabilitation is required afterwards. The rehab period aims to:
- Restore normal Range of Movement to the knee
- Restore normal strength to the muscles around the knee and throughout the lower limb
- Restore good balance and co-ordination during movement
- Maximise muscle balance and motor control during sport specific activities
A post operative protocol will have goals the athlete can progress through before progressing to the next phase. Rehab may progress at different rates. Professional players could expect to return to full sports activity within a six month whereas amateurs are likely to be slower - maybe up to 12 months.
The phases of recovery are broadly summarised as:
- Recovery of range of movement (ROM), normal muscle activity and control of swelling
- Recovery of balance, control and joint position sense
- Recovery of functional movement in weightbearing, walking, jogging and running in straight line
- Exercise against resistance
- Sport specific activities - no contact
- Sport Specific activities - full contact
During the early phases of rehab the opportunity may be taken to work on other parts of the body needing attention i.e. upper body strengthening, core stability
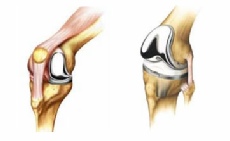
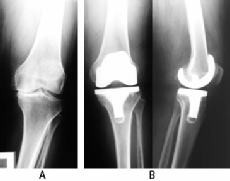
Joints that are severely injured by trauma or that have degenerated significantly may need to be replaced.
There are many types of joint replacement. Anyone having a joint replacement will need some rehabilitation. The protocol for this will depend on a wide range of factors, including
- the joint being replaced
- the type of artificial joint used
- the surgical procedures used
- trauma Vs planned surgery
- age and mobility of person pre-operatively
Some prehabilitation may be indicated to prepare a patient physically for the surgery. This may include an exercise programme to maximise muscle strength and available range of movement, maximise balance and co-ordination, to learn the post operative exercise programme and to ensure good respiratory function.
The rehabilitation following a joint replacement will include basic exercises within 24 hours of surgery and progressively more active exercise during the days after the operation to restore muscle activity and function as quickly as possible.
For joints replaced in the lower limbs this will include getting back on the feet and walking with ‘normal’ gait as soon as possible.
Special attention may be paid to some muscle groups known to be affected adversely by either the deterioration of the joint / the surgery or by special risks – such as possible dislocation of the joints.
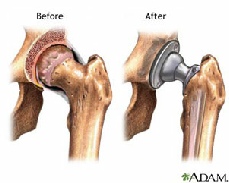
In lower limb joint replacement the important muscle groups for rehab will be the hip extensors and abductors, the knee extensors and flexors and the calf muscles. The key functional activities are walking, step climbing and getting up / down from standing to sitting.
In upper limb joint replacement the key activities are using the hand, shoulder abduction, flexion / extension + rotation, and elbow flexion + extension.
If you would like to discuss rehabilitation following joint replacement please contact us at Ennis Physiotherapy
Clinic for advice




Mon - Fri 9.30am - 8.30pm


3A Barrack Close, Barrack St., Ennis, Co. Clare V95 X437

065 6840757
| Health+Safety Services |
| Sports Clubs+Teams Services |
| Standing Posture |
| Sitting Posture |
| Childhood Posture |
| Using Portable Devices |
| Normal Walking |
| Running |
| Running Drills Videos |
| Muscle Energetics |
| General Fitness |
| Losing Body Weight |
| Gaining Body Weight |
| Weight Loss Programmes |
| Start to Run |
| Start to Swim |
| Start Cycling |
| Start Nordic Waliking |
| Rehab of Tensdons |
| Loading of Tendons |
| Non Specific LBP |
| Posture |
| Intervertebral Disc |
| LBP Treatment |
| Non Specific Neck Pain |
| Neck Care Advice |
| Hamstring Strain |
| Ankle Sprain |
| ACL Injury |
| Joint Replacement |
| Shoulder Dislocation |
| Tennis Elbow |
| Wrist fracture |
| Fractured Knuckle |
| Selecting a Racquet |
| Racquet Grip Size |
| Racuet Sport Injuries |
| Training for Racquet Sports |
| Ski + Board Injuries |
| Injury Videos |
| Injury Prevention |
| Preventing Injury in Musicians |
| Irish Dancing |
| Preventing Dance Injury |
