© Ennis Physiotherapy Clinic, 3A Barrack Close, Barrack Street, Ennis, Co. Clare V95 X437 Tel: (065) 6840757
Spinal Problems Neck + Back Pain Disc Injury Whiplash Posture
Lower Limb Injuries Walking + Running Ligament Injury Snowsports Injury Home Exs Prog
Upper Limb Injuries Ligament Sprains Tendon+Muscle Golf + Bike Set Up Useful Links


065 6840757

Mon - Fri 9.30am - 8.30pm


3a Barrack Close, Barrack St., Ennis, Co. Clare V95 X437
A sprained ankle
ligament occurs when
the foot is twisted
severely, usually
turning inwards under
the leg, either when
turning suddenly or
landing on uneven
ground.
Here is often severe pain, immediate swelling and variable amounts of bruising. If pain on walking or putting weight on the foot persists an X-Ray may be needed to exclude the possibility of a fracture.
Repeated sprains may lead to joint instability and poor balance and co-ordination. Exercises to prevent this should be included in the rehab programme.
Treatment can be provided by contacting us and includes
- RICE Regime
- Proprioceptive support taping / strapping
- Relative rest / reduced activity
- Functional Rehab: jumping, turning, ball drills
- Balance Board exercises
- Calf strengthening
- Progressive jogging / running / jumping / kicking


On this Page
Ankle Sprain Hanstring Strain Muscle Contusion
Anterior Cruciate Ligament Strained Achillles Tendon Joint replacement
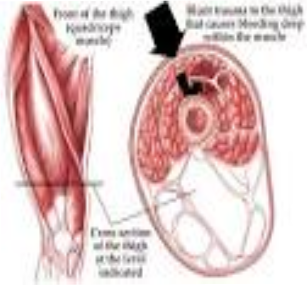
Usually occurring in contact sports when one player accidentally kicks another player, usually on the thigh muscle
The incoming knee crushes the muscle fibres against the
thigh bone causing localised bleeding within and around the
Muscle and possibly bruising + swelling on the thigh.
The injured player usually has
difficulty bending the knee after this injury.
It is critical to avoid causing further bleeding in the 10 days following injury. Severe injury where bleeding is not dispersed and appears as bruising can lead to bone formation within the muscle which is a major complication.
Treatment
RICE Regime with quads on maximum painfree stretch during icing
Gradual return to daily activity - without provoking pain
Massage Therapy after 48 hours min.
Functional Rehabilitation Exercises / restore strength
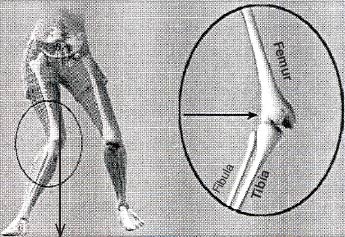
The hamstring group of muscles is regularly injured in sports activities.
Most often it is injured at the end of the leg swing during kicking or as the knee locks straight when accelerating in sprinting.
Hamstring muscles have a number of functions including pelvic positioning / posture and preparing the limb for loading during walking and running.
Risk factors for injury include
Increased tightness in muscle Previous Injury
Reduced flexibility of muscles. Age
Reduced Muscle Strength, Low Back Pain
Treatment
- RICE regime
- Activity without pain, initially with shortened position and
static work (i.e. bridging) gradually increasing in ROM and intensity
- Activation of core
- Lumber movement and leg movements
- Dynamic running without pain or limp: Progress jogging + running,
- Technical drills: sidestepping, hurdle walk over, sumo walk,
lunge, high knee walk, heel flicks
- Gentle Stretching of hamstrings starts after 5 days
- Strengthening programme – general and sport specific

Note:
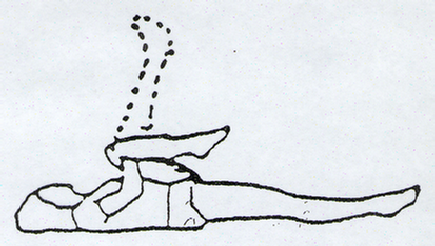
The hamstrings are a group of muscles that extend over two joints and are acting on both joints simultaneously.
They may function differently dependent on the activity where they may either function mostly as a postural or as a dynamic muscle. Thus they are more prone to injury than the quadriceps group which oppose them.
To stretch the hamstring one must have both the hip flexed and the knee extended to achieve a full stretch of the muscle.
In the top picture above the movement is extending the knee with a fully flexed hip, so emphasising stretching the lower end of the muscle while in the lower picture the movement occurs at the hip while the knee is fully extended. This focuses the stretching effect on the upper end of the muscle.
When stretching it is important to support the back of the knee and to avoid hyper-extending the knee, as repeated stretching of the hamstring when the knee is un-supported and hyper-extending can introduce instability into the knee joint. Contact a Chartered Physiotherapist for more advice
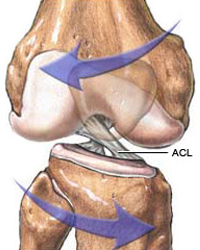
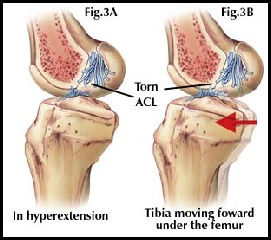
Anterior Cruciate Ligament Injury
The Anterior Cruciate Ligament is a key stabiliser of the knee joint. It particularly prevents the knee from bending backwards too far (hyper-extension) and from bending sideways when the knee moves inwards too much. Injury is very common in sports that require a significant amount of pivoting on one leg while changing direction or where direct contact is likely to occur forcing the knee to bend backwards or inwards. Female athletes are much more at risk of injury when playing or competing at the same level / intensity as their male peers. This is mainly due to the slight differences in anatomical shape of the lower limbs of female - the slightly increased inward slope of the thigh bones making females effectively slightly more ‘knock kneed’.
If the ACL is ruptured it leaves the knee unstable and exposes it increased risk of injury to other tissues in the future. In active sports men and women it is common to reconstruct the ACL during surgery and then undertake a long period of Rehabilitation afterwards. The rehab period aims to
- Restore normal Range of Movement to the knee
- Restore normal strength to the muscles around the knee and throughout the lower limb
- Restore good balance and co-ordination during movement
- Maximise muscle balance and motor control during sport specific activities
Each surgeon generally has a post operative protocol they prefer to be followed and the athlete can progress through the different phases of the rehab at different rates. Professional players could expect a return to full sports activity within a six month period assuming no problems are encountered. Committed amateurs are likely to experience slower progress depending on how much time and effort they can invest in their recovery.
The phases of recovery are broadly
- Recovery of range of movement (ROM), normal muscle activity and control of swelling
- Exercise for recovery of balance and proprioception - joint position sense
- Recovery of functional movement in weightbearing, walking, jogging and running in straight line
- Exercise against resistance
- Sport specific activities - no contact
- During the early phases of rehab the opportunity may be taken to work on other parts of the body needing attention i.e. upper body strengthening, core stability etc


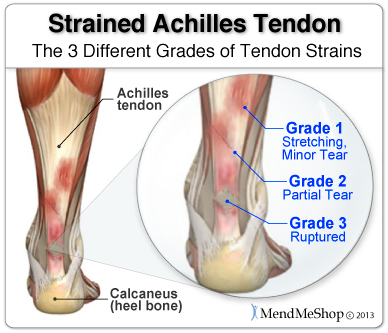
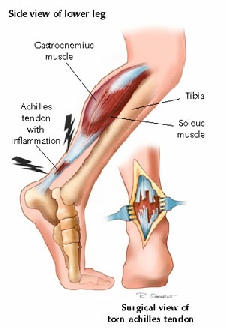
Achilles Tendonitis / Tendonosis
Achilles tendon injury occur very frequently amongst all populations. An acute tendon injury that is acutely inflamed is referred to as a tendonitis and a more chronic injury where no inflammation is present is referred to as a tendonosis.
Overuse tendonpathy is usually associated with gradual onset of pain and morning stiffness after and increase in activity. Symptoms diminish with activity levels but return several hours afterwards. Heat also is reported to alleviate symptoms.
Acute onset of symptoms is usually associated with partial tears of the tendon but may also occur with complete rupture. In the latter case people often report the feeling of being struck or kicked on the heel / tendon and of hearing a loud ‘shot’ like noise. There is often thickening in the area of the tendon that is affected and a sensation of creaking during movement. Other factors that need to be considered are foot mechanics, tight calf muscles, weak calf muscles, poor balance, stiffness at the joints of the ankle + foot and an ability to single leg heel raise / hop.
Injury in sports people is often associated with changes in intensity of training or sudden increases in training loads. In a general population it may be associated with sudden changes in general activities or in footwear, a change to little or no heel or support / walking barefoot (as in on holidays)
Treatment as provided at Ennis Physio Clinic includes
Treatment is primarily aimed at restoring the tensile strength of the tendon to that of pre injury levels. Where there is inflammation present this must be controlled and eradicated and the healed tendon then rehabbed.
In the acute phase the RICE regime is implemented and rest from aggravating activities and ice for swelling are used.to minimise pain and tenderness.
Gradual increase in the loading on the tendon during activity is begun as soon as pain and other symptoms allow, and are not exacerbated by.
Simple heel raise both concentrically and eccentrically - raising up onto the tippy toes and down onto the heel slowly and controlled - are begun as soon as possible and integrated into normal functional activities wherever practice.
Gait re-education and stepping practice without a limp is commenced and achieved prior to progressing to walking fast, striding, jogging, running and jumping. Slow heel raises are progressed to rapid heel raises, rapid alternate heel raising, hopping, skipping and then jumping. Acceleration is practiced in a controlled manner - changing walking and / or running speeds. A variety of walking and running drills are available if needed.
Treatment can vary in terms of duration depending on severity of injury and the demands you intend to place on your healed tendon. The following video gives an indication of some but not all of the treatment possibilities. Please note reference to Physical Therapy I/ therapists n the USA is the equivalent to a Chartered Physiotherapist in Ireland.
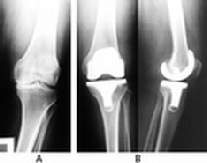
Joints that are severely injured traumatically or that have degenerated significantly may need to be replaced entirely. There are many different types of replacement joints and different surgical approaches. The most suitable option is selected for each individual case by the orthopaedic surgeon. All persons undergoing joint replacement surgery will undergo some rehabilitation post operatively and again the exact details will depend on a wide range of factors which may include the joint being replaced, the type of artificial joint used and the surgical procedures used, trauma Vs planned surgery, age and mobility of person pre-operatively etc.

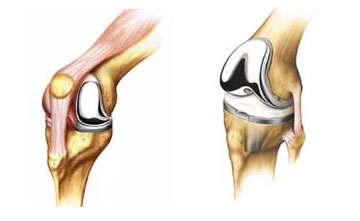 Typically if a joint replacement is planned in advance the person may be recommended to undergo some prehabilitation in order to have them prepared physically to get over the surgery. This may include an exercise programme to maximise muscle strength and available range of movement, maximise balance and co-ordination, to learn the post operative exercise programme and to ensure good respiratory function.
Typically if a joint replacement is planned in advance the person may be recommended to undergo some prehabilitation in order to have them prepared physically to get over the surgery. This may include an exercise programme to maximise muscle strength and available range of movement, maximise balance and co-ordination, to learn the post operative exercise programme and to ensure good respiratory function.
The rehabilitation following a joint replacement will include some basic exercises within 24 hours of surgery and progressively more active exercise during the days after the operation which will restore muscle activity and function as quickly as possible. For joints replaced in the lower limbs this will include getting back on the feet and walking as soon as possible and getting back to an independent unsupported ‘normal’ gait pattern as soon as possible.
Special attention will be paid to particular muscle groups that are known to be affected adversely by the arthritis / degeneration of the joint / surgery and special risks – such as possible dislocation of the new hip during certain activities – identified for each person.
In lower limb joint replacement the main muscle groups considered will be the hip extensors and abductors,
the knee extensors and flexors and the calf muscles and the key functional activities of walking, step climbing
and getting up / down from standing to sitting. In the case of upper limb joint replacement the key activities
will be using the hand and shoulder abduction, flexion / extension and rotation and elbow flexion + extension.
If you would like to discuss rehabilitation following joint replacement please contact us at Ennis Physiotherapy
Clinic for advice