© Ennis Physiotherapy Clinic, 3A Barrack Close, Barrack Street, Ennis, Co. Clare V95 X437 Tel: (065) 6840757
Spinal Problems Neck + Back Pain Disc Injury Whiplash Posture
Lower Limb Injuries Walking + Running Ligament Injury Snowsports Injury Home Exs Prog
Upper Limb Injuries Ligament Sprains Tendon+Muscle Golf + Bike Set Up Useful Links


065 6840757

Mon - Fri 9.30am - 8.30pm


3a Barrack Close, Barrack St., Ennis, Co. Clare V95 X437
What Is Physiotherapy?
Physiotherapy is a therapeutic profession concerned with restoring well-being to people following injury, pain or disability, by using mainly physical means such as exercise, manipulation, mobilisation, massage and electrical modalities. In this way it helps patients achieve their full physical potential.
Traditionally, physiotherapy was regarded as being rehabilitative but increasingly the profession has expanded to include preventative and educational roles, drawing on expertise in the fields of anatomy, physiology, biomechanics, ergonomics and normal movement.
What Is A Chartered Physiotherapist?
The title "Physiotherapist" alone is not evidence of a formal qualification in Physiotherapy. The title "Chartered Physiotherapist" and the initials MISCP indicate that a physiotherapist is a member of the Irish Society of Chartered Physiotherapists. After Sept 2018 the profession will be regulated by CORU on behalf of the state.
Chartered Physiotherapists are recognised by the medical professions, and the Department of Health, as being university degree qualified and being committed to continuing education and research.
A physiotherapist can assess the problem, provide treatment, help you understand your problem and get you back to your normal activities as soon as possible.
Welcome to our ‘Useful Information’ page.
On this page you can find some basic information on the following:
What is Physiotherapy and What is the Role of Physiotherapist
Immediate Care of Sports Injury Posture

Fees
Per Session €50
Duration: 1 hour approx
Chartered Physiotherapy fees can be reclaimed, in part or in full, from health insurance providers such as VHI, Laya Healthcare, Aviva Health, ESB + Garda Medical funds depending on the policy terms and conditions.
Tax relief may be claimed by filling in the Med1 form available from the Revenue Commissioners at www.revenue.ie
Postural strain is a common factor and cause of spinal discomfort for many people. ‘Normal’ posture is develops during childhood and young children generally have good postural habits.
Poor postural habits can occur at any time but generally become habitual during or after teenage years. The selection of age appropriate and height / size appropriate furniture and equipment for work or leisure is crucial for encouraging good posture. However even the best ergonomically designed furniture and equipment can be used badly and therefore is not a guarantee of good posture.
An example of this is seating - even with an appropriate chair which provides adequate support in the right places a person may sit poorly. If the seat is too low (hips below the knee level) or the seat is too deep (thigh is too short and can’t meet the backrest) the pelvis will roll backwards into posterior tilted posture and the spine must flex which places pressure on the discs and on the posterior spinal ligaments/joint capsules. Raising the seat level / providing additional support directly behind the spine may alleviate this type of problem.
Good overall body posture can be achieved when the eyes are held level and facing forward, the shoulders are level, the spine is straight and centrally aligned, the pelvis is held in neutral and where there is relative muscle balance around the pelvis and shoulder girdle areas.
Each segment of the body and each joint can also have a ‘preferred’ or ergonomically sound posture depending on the activity being undertaken and generally refers to the position in which the body can operate with most effectiveness and efficiency and least risk.
For more detailed information relating to posture please see the posture information page.
Common causes of sports injuries are:
- Inadequate and/or inappropriate fitness and preparation for sport
- No Warm-up exercises done.
- Proper post-exercise cooling down is skipped.
- Inappropriate training - doing too much and repeating the same activities
- Pain during or after exercise being ignored.
- Improper equipment – wearing the wrong type of sports shoes.
- Incorrect technique and posture
- Collision, notably in contact sports such as rugby
- Insufficient rehabilitation and returning to sport too soon following an injury
Immediately after an injury use The ‘P.R.I.C.E.’ Protocol for self treatment
- Protect – the injured area
- Rest – the damaged area to avoid further injury.
- Ice – for 5-10min initially + 20-30min during the first 5 days
- Compress – the injured area to minimise swelling and aid recovery
- Elevate – the injured area to prevent the accumulation of fluid.
Post Exercise Recovery Strategies
- Keep walking after you finish your race for 5-10 minutes to help prevent joint stiffness and muscle tightness
- Ensure you change into a warm set of clothes as soon as possible
- Eat a high carbohydrate + protein snack within 30 minutes after completing your race. Eat a balanced meal within 2 hours after your race and rehydrate adequately
- Spend 10-20 minutes doing static stretches to prevent the onset of muscle soreness over the following days
- Soak your body in a cold bath (ice bath), lake or ocean within a few hours of your race. This aids in decreasing inflammation in the working muscles, thereby aiding recovery
- Foam Rolling can be used to self-release tight muscles post race
- A massage in the week following your race will aid your recovery and reduce muscle tightness.
- Allow time for your body to recover before returning to training.
Consult a Ennis Physiotherapy Clinic if you have pain or niggles that do not settle within a few days. Post injury.
Assessment is the process by which a physiotherapist evaluates a person that presents to them for treatment. There are a number of elements to the overall assessment. The process can be divided into the subjective examination, during which is what the person tells the physiotherapist about the problem they are presenting with, and the objective examination which is where the person is examined by the physiotherapist. A variety of approaches and techniques can be used during either of these elements of the assessment. But the key points are summarised below.
Subjective Examination
This is what the person tells the physiotherapist about the problem they are experiencing and how it is affecting them. The physiotherapist may ask some probing questions to illicit information that they need in order to make a better evaluation of the problem. Physiotherapists generally prefer to get first hand information directly from the patient themselves but where this is not possible it is also possible to seek input / information from other people close to the patient or who may be able to communicate on their behalf. Some of the information likely to be sought by a physiotherapist include
- What exactly are the symptoms (pain / stiffness etc)
- Where in / on the body are the symptoms felt
- What is the nature of the symptoms (sharp / Dull etc)
- What Aggravates or eases the symptoms
- When do the symptoms occur (am/pm/night)
- How did it start
- Has it progressed
- Are there any other issues
- Are there any other medical conditions
- Is there any (daily) pattern to the symptoms
- How do activities of daily living affect the symptoms (work, leisure and home life
- How does rest affect the symptoms
Objective Examination
The objective examination is what the physiotherapist can determine from the actual examination testing of the patient and in particular the affected areas, or areas thought to be affected. There are standard testing procedures for objective testing different functions of the musculoskeletal system.
Testing during the objective examination may include
- Posture
- Active range of movements of the joints
- Passive range of movement of the joints
- Muscle strength
- Ligament stress testing
- Both the amount and the quality of movement is assessed + recorded.
- Activity specific movements may be assessed (sports / work specific task) are often included.
Neurological testing of
- Reflexes
- Neural tension / mobility
- Sensation -(light touch, heat, cold)
- Proprioception / joint sense
- Balance / Co-ordination
- Hand or foot -eye co-ordination
Assessment of Gait - pattern, quality of movement, symmetry
- Provocative testing if necessary - if difficult is experienced in reproducing the symptoms
- Quick Tests
- Exclusionary Testing
Reaching a medical diagnosis is the process of identification of the nature and cause of a condition. It uses knowledge, logic, analytics, and experience to determine which disease or condition is causing a person's signs + symptoms.
The foundation of diagnosis is always the information from the history and the physical examination, but often one or more diagnostic procedures, such as x ray or MRI, may also be used to assist in making or to confirm the diagnosis.
Diagnosis is often challenging because the signs and symptoms can be nonspecific and atypical for a particular condition. Thus a differential diagnosis, where several possible explanations are considered, is used to determine the most likely correct answer.
Diagnostic opinion can take many forms - naming the disease, lesion, dysfunction or disability or may indicate the degree of abnormality on a continuum or a kind of abnormality within a classification. It is generally subject to constant review based on response to treatment provided.
Prognosis is the likely course of a medical condition. It is an opinion, based on medical experience, of the likely course of a medical condition. In effect it is a forecast of the likely outcome of a condition based on the information to hand at that time. In some cases it can be very accurate and expressed with confidence whereas in others it may be less certain. It may be more difficult to apply research findings to an individual patient as often there is a multitude of factors which can impact on the outcome.
These factors include factors relating to the condition itself, the availability of the most appropriate or best treatments and the environment it can be provided in, factors relating to the patient including their compliance with treatment, their health status etc.
A complete prognosis includes the expected duration, the function, and a description of the course of the disease, such as progressive decline, intermittent crisis, or sudden, unpredictable crisis.
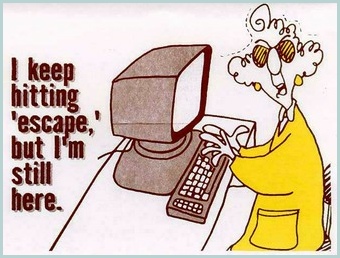
A Physiotherapist can provide a variety of treatments such as
- Manipulation,
- Massage,
- Electrotherapy,
- Functional Rehabilitation exercises,
- Advice on
- The cause of your problem
- Return to your normal activities
- Prevention of pain returning in the future.
 Exercise is the most important way that you can:
Exercise is the most important way that you can:
- ease stiffness and pain
- build up muscle strength and stamina
- improve your flexibility and general fitness.
- improve co-ordination
- address muscle imbalance issues
These benefits continue for some weeks after the pain and symptoms subside so it is advisable to persist with the exercises for a period after the pain has gone.
Consult Ennis Physiotherapy Clinic if you need an assessment, treatment or advice about your back pain especially if it has not settled within a few days
Where an identifiable hazardous circumstance is present that expose a person to increased risk of musculoskeletal injury, a physiotherapist will aim to minimise that risk. Such circumstances may include some or any of the following non -exhaustive list
Intrinsic Factors Extrinsic Factors
Strength Footwear / Clothing
Endurance Work / Sports Equipment
Co-ordination Work / Sports Furniture
Balance Activities (Design / requirements / loading)
Flexibility / Deformity Location (outdoor / indoor / vehicular)
Awareness Repetition / rest periods
Experience Loading on body (weights / postures / vibration)

The main factors to consider are seat height, saddle fore / aft position and arm reach.
The cyclist should be warmed up when setting up the bike.
The seat height is correct when the pedal crank is in line with the rear tube of the frame and:-
1. The pelvis is level
2. The knee is at 250-300 off fully extended and
3. The foot is parallel to the floor (neutral at ankle).
The knee is fully extended at the bottom of the pedal stroke.
This position will be the distance from the top of the saddle to the centre of the bottom bracket along the line of the
back tube of the frame or the inside leg seam measure x 0.88 A number of additional factors need to be considered to to fine tune final seat height.
Too high a seat gives less power, stresses the hamstring and calf muscles and excessive hip extension destabilises the pelvis.
Too low a seat increases pressure on the knee cap joint and is less effective for the muscles.
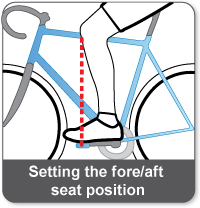
The fore / aft position of the saddle is important for knee loading. The correct position is where the front of the knee is vertically above the centre of the pedal axis.
A number of factors affect the final position including event type, rider size, hip flexibility and bike stability/handling.
Some riders like a slightly forward tilted saddle.
Saddles that are too forward cause increased compression forces at the knee joint, knee flexion and hip extension.
Muscle length becomes less optimal.. Too far back and the hamstring and gluteal muscles are over lengthened and
become less efficient.
The Reach position of the handlebars is affected by a number of factors.
Good positioning is achieved when the pelvis is anteriorally (forward) tilted, a flat back between hips and shoulders,
unlocked elbows with relaxed arms and shoulder (blades) retracted in neutral.
Fine adjustments can be made to take account of the position of feet, cleat position, crank length, type of handlebar
and seat, aerodynamic position and pedaling technique. Always seek professional advice for bike fitting
A golf club connects the player’s body and the golf ball. The club should be well suited to the player and their swing dynamics. If the club is not sized or used correctly the player must ‘compensate’ for this and the risk of injury is increased. The correct club selection allows the player to perform an effective, efficient and consistent shot. NB A righted player is assumed here
Shaft length: Standard club size is based on male (178 cm) and female (163 cm) height and the standard iron shaft length for males is approx 96 cm and a female is 93 cm. The driver length is 109 cm and 103 cm respectively. Graphite clubs, being lighter, are usually longer by 2.5cm. A longer shaft has more flex and vice versa.
A number of methods are used to determine correct shaft length. ‘Knuckle Height’ is often used to determine the correct shaft length. Standing upright, with the hand by the side (closed fist), measure from the floor to the knuckle of the left middle finger. Retail outlets will have tables so the correct size of club can be selected
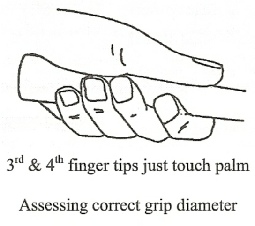 Grip size: A number of methods may be used. When the club is held by the left (top) hand. With the correct grip size the tips of the 3rd and 4th fingers should just touch the thumb side of the palm.
Grip size: A number of methods may be used. When the club is held by the left (top) hand. With the correct grip size the tips of the 3rd and 4th fingers should just touch the thumb side of the palm.
Extra layers of grip tape may be used to increase the grip size by 1 mm approx with each layer if necessary.
A grip that is too large is less efficient and effective and can cause increase muscle tension increasing the risk of tennis/golfers elbow and wrist tendonitis. An excessively small grip increases joints sprain and can lead to pain and arthritis.
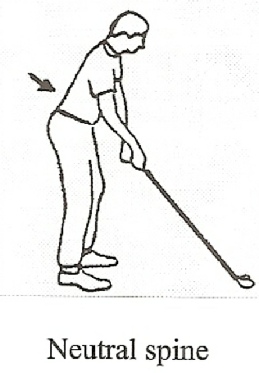
Set-up stance / Address Posture: This can lead to an effective dynamic swing and ball strike. The knees should be bent 25-300. The trunk should also be bent forward 25-300 with the spine aligned straight between the hip and shoulder level. The bottom should feel slightly stuck outwards behind.
 Dynamic Elements of Golf Club Sizing
Dynamic Elements of Golf Club Sizing
During the golf swing the club will flex and twist thereby changing the position and attitude of the club head at the point of contact.
Lie Angle: At stance the toe of the club head should be slightly raised relative to heel.
With increasing club head speed during the swing the club flexes downwards so that at contact with the ball the sole of the club head should be parallel with the ground.
Contact near the heel of the club head mean the lie angle is too small and causes the club face to become more closed and will generally pull the ball to the left, similar to what occurs with too flat a swing plane or a shaft that is too long.
Contact near the toe of the club head may cause the opposite to occur.
Club Head Speed / Torque: This will affect the flex occurring within the shaft of the club during the golf swing. The faster the head speed the greater the flex.
The amount of torque or twist occurring in the club during the swing will determine the degree to which the club face is open or closed at contact and thus will determine which direction the ball will travel
Disclaimer
All advice provided on this website is general in nature and is for information purposes only.
It is not intended to replace assessment or treatment by a Chartered Physiotherapist or other healthcare professional.
If you have any doubt about whether it applies to, or is appropriate for you, you should contact your
Chartered Physiotherapist or GP for clarification.
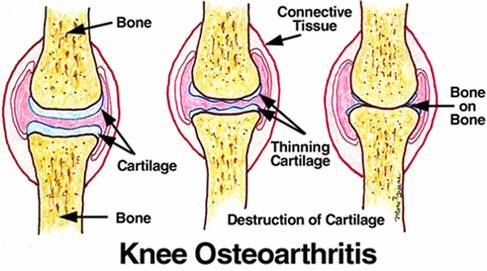
The ends of the bones at the joints are covered with cartilage. This cartilage allows minimal friction during movement between the bones. The surface is normally very smooth and is wetted by synovial joint fluid which further reduces friction during movement. The cartilage does not have its own blood supply and therefore is poorly able to heal once injured. Pressure of body weight or use will compress the cartilage when the joint is under loading and some joints take more pressure – such as the spine and lower limbs joints – than others.
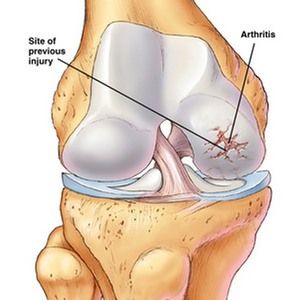
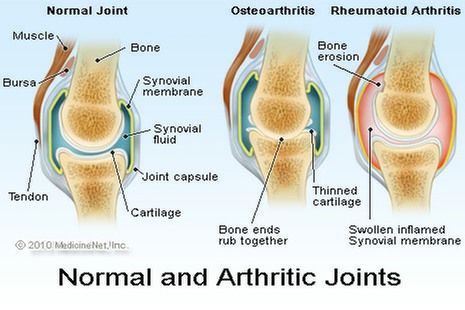
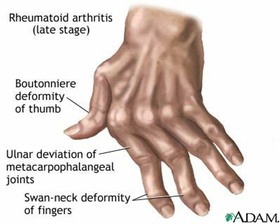
Arthrosis refers to the process of normal aging within the joints which cause changes in the cartilage and the underlying bone. This is often referred to as ‘wear + tear’ or ‘degeneration’ at the joint. The smooth surface becomes softened and begins to show signs of tiny splits or cracks. As the condition progresses these cracks become more extensive, longer and deeper causing the surface to become increasingly uneven. When the cracks extend through to the bone, the bone will begin to change by becoming ‘harder / more dense and starts to become enlarged. During this process the person may be unaware of it in the earlier phases but later become aware of a deep bony ache, creaking or grinding of the joint during movement (crepitus) and increasing stiffness after rest periods. When advanced the joint may become deformed or mis-aligned, unstable and restricted in range of available movement
Arthritis refers to a degenerative joint which becomes inflamed as a result of an additional insult such as a sudden twist, excessive loading, overuse etc. There may be swelling and in addition to the other symptoms above.
The process of degeneration is not reversible so the damage, some of it normal age related wear, within the joint surfaces must be managed proactively wherever possible. Steps can be taken from an early age to ensure the degree and rate of deterioration of the joint surface is minimised by using good postures, avoiding excessive overuse and abnormal positions / loading, by maintain good movement patterns and maintaining good strength.
Once deterioration is detected or felt then the joint should be protected where possible, muscle strength should be maintained. Good posture maintenance and proactive treatment of signs + symptoms as they arise is recommended. Reducing the loading or pressure on the joints may include using a walking stick / crutches may be helpful as well as reducing overall body weight.
There is a whole range of inflammatory arthritis conditions such as rheumatoid arthritis and juvenile arthritis which require ongoing medical and specialist treatment. For more specific advice about any arthritic joint please contact us at Ennis Physiotherapy Clinic where we will be happy to assess + treat it as necessary.