|
Unreactive to Light |
Pupil Reactivity Score |
|
Both Pupils |
2 |
|
One Pupil |
1 |
|
Neither Pupil |
0 |
Graduated Return to Play (GRTP)
Disclaimer
If you have any concern about someone who may have been concussed and has developed signs and symptoms later you should immediately seek medical attention or attend the Emergency Department.or GP.
Concussion is the most common type of minor head injury.
It involves a minor traumatic brain injury (TBI). Concussion usually has transient signs + symptoms that can include headaches, impaired concentration, memory, balance and coordination.
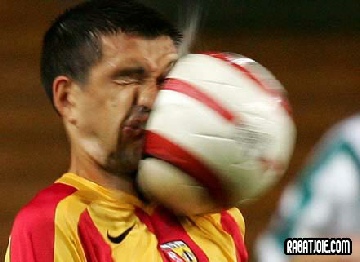
Head injuries are common and can happen in a variety of ways, i.e. through falls, car accidents, sports and assault that result in a bump, blow, or jolt to the head head (or a hit to the body) that causes the head, and the brain within, to move rapidly back and forth.
Violently shaking the head and upper body also can cause concussions.
This sudden movement can potentially cause the brain to bounce around or twist within the skull, creating chemical changes in the brain and sometimes stretching and damaging brain cells.
There may not be obvious signs and symptoms immediately after the injury but some may appear in the days and months afterwards.
Most people normally recover fully following a concussion.
Some concussions may cause loss of consciousness but most do not. It's possible to be concussed and not realise it.
Concussions are particularly risk of participation in a contact sport.
A concussion can present with a range of signs + symptoms, depending on the severity of the injury sustained. Most are minor but some can cause severe brain damage.
Concussions can be graded as being:
- Mild (grade 1)
- Moderate (grade 2)
- Severe (grade 3),
The grading is dependent on factors such as loss of consciousness (LOC), amnesia, and loss of equilibrium. Any LOC is a Grade 3 event.
The signs and symptoms of a concussion can be subtle and may not be immediate. Symptoms can last for days, weeks or even longer.

Common signs and symptoms after a concussive traumatic brain injury are set out below. Loss of memory (amnesia) and confusion are common. The amnesia usually includes forgetting the event that caused the concussion.
People who show the signs + symptoms listed below, or simply say that they just “don’t feel right” after a bump, blow, physical contact or jolt to the head or body, may have a concussion or an even more serious brain injury. The risks associated with concussion are sufficient to require that they should be monitored carefully until it is no longer necessary. If they have LOC or severe injury they should seek medical attention.
These are things that other people can observe or see in the injured person. The ‘injured’ person may exhibit some or all of the following. They…
- Lose consciousness (LOC)
- Can’t recall events prior to or after a hit or fall.
- Appear dazed or stunned.
- Vomiting
- Forget an instruction, are confused about an assignment or position, or are unsure of the game, score, or who the opponent is.
- Slurred speech
- Move clumsily.
- Answer questions slowly.
- Have lost consciousness (even briefly).
- Show mood, behaviour, or personality changes.
These are things that the ‘injured’ person complains of or reports. They may report simply ‘not feeling right’.
In most people, symptoms occur within the first seven to 10 days and go away within three months. Less often they can persist for a year or more
Concussion symptoms fit into four categories:
- Thinking and remembering.
- Physical.
- Emotional and mood.
- Sleep.
They may complain of….
- Headache or “pressure” in head
- Loss of memory – especially of the impact / event
- Being confused
- Nausea or vomiting.
- Balance problems or dizziness
- double or blurry vision. ‘Seeing stars’
- Being bothered by light or noise.
- Ringing in the ears
- Feeling sluggish, fatigued, hazy, foggy, or groggy
- Being confused, or of impaired concentration or memory problems
- Sleep disturbances
- Psychological adjustment problems and depression
- Disorders of taste and smell
- Just not “feeling right,” or “feeling down”.
Concussion Signs
Concussion Signs
Head trauma is very common in young children. But concussions can be difficult to recognise in infants and toddlers because they can't describe how they feel. Concussion clues may include:
- Appearing dazed
- Listlessness and tiring easily
- Irritability and crankiness
- Loss of balance and unsteady walking
- Crying excessively
- Change in eating or sleeping patterns
- Lack of interest in favourite toys
Symptoms in Children
There are six types described, identified by the signs + symptoms they exhibit:
- vestibular (balance issues);
- ocular (vision problems);
- Mood
- anxiety,
- migraine headaches, and
- cervical (problems with the neck).
Signs and symptoms generally show up soon after the injury. However, some may have delayed onset over hours or days, making it difficult to establish the severity of the injury to the brain.
Therefore close monitoring is required over the following hours and days for evolving signs + symptoms.
The goal of treatment after concussion is to effectively manage your symptoms. If signs and symptoms are worsening you should always attend A+E or to your GP.
Types of Concussion
This document was developed out of consensus among world experts in medicine and in sport.
I t sets out ‘11 Rs’ of SRC management of concussed players. The sections are: Recognise; Remove; Re-evaluate; Rest; Rehabilitation; Refer; Recover; Return to sport; Reconsider; Residual effects; Risk reduction.
t sets out ‘11 Rs’ of SRC management of concussed players. The sections are: Recognise; Remove; Re-evaluate; Rest; Rehabilitation; Refer; Recover; Return to sport; Reconsider; Residual effects; Risk reduction.
This statement should be considered alongside the Concussion Recognition Tool (CRT5), the Sports Concussion Assessment Tool (SCAT5) or the Child SCAT5.
The 5th Concussion Consensus Statement
Sport Related Concussion (SRC)
Assessment + Management of Concussion
|
Motor |
|
|
Obey Commands |
6 |
|
Localising |
5 |
|
Normal Flexion |
4 |
|
Abnormal Flexion |
3 |
|
Extension |
2 |
|
None |
1 |
|
Verbal |
|
|
Orientated |
5 |
|
Confused |
4 |
|
Words |
3 |
|
Sounds |
2 |
|
None |
1 |
|
Eyes |
|
|
Spontaneous |
4 |
|
To Sound |
3 |
|
To Pressure |
2 |
|
None |
1 |
Glasgow Coma Scale
The Maddock’s questions are used for assessing orientation in time and place in possible concussion / head injury. The SCAT (Sport Concussion Assessment Tool) includes the following modified Maddock’s questions in the pitch side assessment of a possible concussion. The Maddock’s questions should be preceded with the preface: "I am going to ask you a few questions, please listen carefully and give your best effort."
At what venue are we today?
- Which half is it now?
- Who scored last in this match?
- What did you play last week?
- Did your team win the last game?
The Maddock’s questions are used as part of the clinical assessment of possible concussion on the sports side line along with other assessments described in SCAT. Because the Maddock’s questions can be asked by anyone, they are valuable during sports events where no health care professional trained in performing a full side line screening for concussion is present, as is often the case in the amateur game.
if an athlete answers all the Maddock’s questions correctly then the likelihood that he is suffering from concussion is low although the Maddock’s questions only form one part of the SCAT which also includes a combination of other diagnostic tools
Maddock’s Questions for Children
Because children under the age of 13 do suffer concussion and respond to questions differently, the SCAT calls for a child aged 5 to 12 years to be asked four simple questions to determine orientation to time and place:
- Where are we now?
- Is before or after lunch?
- What did you have last lesson/class?
- What is your teacher's name
Maddock’s Questions

There is a distinction between the management of amateur and professional / elite level players who have professional support structures available to them on a regular basis.
For instance World Rugby advocates a ‘Recognise+ Remove” Policy for amateurs and the ‘Head Injury Assessment (HIA)’ protocol for the elite game. Other sports bodies produce similar type of protocols for their sports with slight variations i.e. FIFA, GAA etc
World Rugby’s‘Recognise and Remove’ incorporates 6 of the 11 ‘R’s
- Recognise -
Know the signs and symptoms of a concussion so you understand when an athlete might have a concussion.
- Remove -
If an athlete has a concussion, or even a suspected concussion, he or she must be removed from play immediately.
- Refer -
The player should be referred immediately to a qualified healthcare professional who is trained in evaluating and treating concussions.
- Rest -
Players must rest from exercise until symptom-free and then start a Graduated Return to Play. - Slower for children and adolescents.
- Recover -
Full recovery from the effects of a concussion is required before return to play is authorized. This includes being symptom-free.
- Return -
For a safe return to playing rugby, a player must be symptom-free and cleared to play in writing by a qualified healthcare professional, The player must complete the GRTP (Graduated Return to Play) protocol.
Graduated Return to Play (GRTP)
T
In Elite level games (Professional + Test level) a player who requires an HIA:
- Leaves the field of play; and.
- Is temporarily replaced (even if all the replacements have been used).
- The game cannot restart until the player who requires an HIA has been temporarily replaced.
The HIA is a series of checks used to determine
- whether or not an athlete is suffering from concussion and
- whether they may, or may not, return to the field of play.
The Head Injury Assessment (HIA) Protocol is a three-stage process to assist with the identification, diagnosis and management of head impact events with the potential for a concussion.
- Stage 1 – game day, off field assessment using the HIA1 Form
- Stage 2 – post-game, same day assessment using HIA2 Form
- Stage 3 – 36-48 hour post-injury assessment using HIA3 Form.
When there is a suspected incident of head impact the player(s) involved must be removed, either permanently or for further assessment.
Players displaying obvious on-pitch signs of concussion must be immediately and permanently removed from play, without further assessment.
When not showing clear on-pitch symptoms or signs, players must undergo an off-field assessment (HIA1) consisting of a clinical evaluation by an attending doctor who is aided by screening tools and video reviews. Players cannot return until 10 minutes for assessment has elapsed. Players taken off for HIA can be replaced, and any replacement can take a kick.
The off-field HIA1 screen has four components and they are:
- 12 immediate and permanent removal criteria (known as Criteria 1 indications) AND
- an off-field screening tool AND
- pitch-side video review AND
- clinical evaluation by the attending doctor
After the match any player entered into the HIA protocol must undergo another evaluation within three hours (HIA2). This is a check of symptoms, memory assessment and balance evaluation – compared with previous individual players baselines - and confirms early diagnosis of concussion as well as monitoring clinical progress after the injury..
36-48 hours post injury (after 2 nights rest), the player(s) will be assessed again (HIA3), going through a symptoms check-list, balance testing and a cognitive assessment tool like CogSport or Impact. This screening will identify any late concussion.
A post-game video review process will identify if further education and training for the players or club personnel is recommended
Elite Player (HIA)
Head Injury Assessment

In Soccer the FA in the UK have produced a guidance document for dealing with concussed players and this includes guidance on Graduated Return To Play in both standard care (amateur game), and in enhanced care circumstances (professional game) where significant medical and paramedical professional are available to monitor the return to play over a shortened time frame.
There are many levels of consciousness, ranging from normal consciousness to a deep coma. The Glasgow Coma Scale (GCS) is used as a measure of the level of consciousness of a person who has had a head injury – including those with concussions. This scale is useful in deciding about treatment for the injured person
The scale measures 3 aspects of consciousness:
- eye-opening,
- verbal response (i.e. speaking) and
- responsiveness of the body (i.e. to pain).
The person's score in each area is added up to give a maximum score of 15 (normal consciousness) and a lowest level of 3 (severe coma). A separate scale is used for assessing babies + children, and allowances must be made for those with dementia / learning disability as these reduced abilities may impact on their GCS scores
The scoring on the scale is set out as below
Minor Brain Injury 13-15/15
Moderate Brain Injury 9-12/15
Severe Brain Injury 3-8/15
Glasgow Coma Scale Pupils Score (GCS-P)
The Glasgow Coma Scale provides a clinical index of the ‘overall’ acute impairment of brain function, or so called ‘conscious level’. The GCS Pupils Score (GCS-P) was constructed to bring together information about a patient’s responsiveness as reflected in the GCS Score and the pupil reaction which indicates brain stem dysfunction
The Pupil Reactivity Score reflects loss of pupil reactivity to light and is calculated as follows.
The GCS-P is calculated by subtracting the Pupil Reactivity Score (PRS) from the Glasgow Coma Scale
CS-P = GCS - PRS
© Ennis Physiotherapy Clinic, 3A Barrack Close, Barrack Street, Ennis, Co. Clare V95 X437 Tel: (065) 6840757
Spinal Problems Neck + Back Pain Disc Injury Whiplash Posture
Lower Limb Injuries Walking + Running Ligament Injury Snowsports Injury Home Exs Prog
Upper Limb Injuries Ligament Sprains Tendon+Muscle Golf + Bike Set Up Useful Links


065 6840757

Mon - Fri 9.30am - 8.30pm


3a Barrack Close, Barrack St., Ennis, Co. Clare V95 X437